Gut health is the foundation of our immune system. The stronger our body’s ability to digest and extract nutrients, the stronger our immune system’s defense against infections. In this article, we will get a bit of a deeper understanding of the role of the microbiome and how we can improve IBS symptoms over time by supporting intestinal diversity.
What is Irritable Bowel Syndrome (IBS)?
Irritable bowel syndrome (IBS) is a chronic disorder of the gastrointestinal tract. It is characterized by abdominal pain and bowel habits alternating between constipation and diarrhea (1). IBS impacts approximately 12% of North Americans and generally is diagnosed in individuals less than 50 years of age (2). Patients with IBS suffer not only from gastrointestinal discomfort, but approximately 40–60% experience psychological disorders, such as depression or anxiety (3). Not surprisingly, IBS has been shown to negatively impact one’s quality of life, as well as to adversely affect society’s financial resources.
It’s difficult to determine how an individual develops IBS. However various studies have been conducted across the globe to better understand the etiology. The results indicate that the etiology is multifactorial and includes altered brain-gut interactions, genetic predispositions, dysbiosis and/or environmental factors, such as diet (4).
So let’s talk about gut bacteria.
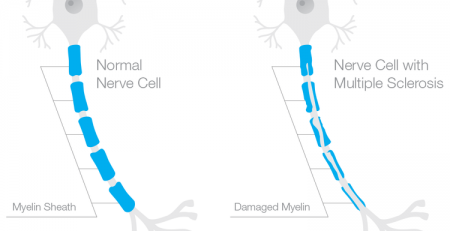
The human body is full of bacteria. We, in fact, have more bacteria cells than we have human cells. Our bodies contain trillions of microorganisms — outnumbering human cells by 10 to 1. These bacteria live all over our bodies, including on our skin, inside the nose, in the throat, in the mouth, in the vagina, and in the gut. The majority of the bacteria found in the body live in the gut. According to research, the richer and more diverse the community of gut microbes are, the lower your risk of disease and allergies. Most of the bacteria in our gut have a positive effect on our health but when one of these bacterial colonies is out of balance, it can lead to dysbiosis, a microbial imbalance.
In 2012 a Human Microbiome Project (HMP) was developed to study the genetic code of bacteria, to better understand the correlation of disease and the microbiome. “Humans don’t have all the enzymes we need to digest our own diet,” said Lita Proctor, Ph.D., HMP program manager. “Microbes in the gut break down many of the proteins, lipids and carbohydrates in our diet into nutrients that we can then absorb. Moreover, the microbes produce beneficial compounds, like vitamins and anti-inflammatories that our genome cannot produce” (5). Individuals with IBS are known to have reduced microbial diversity compared to healthy individuals (6). That’s why one of the ways to support health in individuals with IBS is to ensure we support gut health. If we can improve the microbial diversity, food is better digested and in turn symptoms of IBS reduced.
So how does food play into all this?
Food choices seem to be the most significant triggering factor for IBS symptoms. Food choices in fact may be one of the factors that could have led someone to develop IBS in the first place, as the food we consume directly influences the composition of our microbiota (7).
Research looking at diet shows that those consuming a traditional diet, rich in fermented foods, have significantly lower levels of depression and anxiety (25-30%) and symptoms related to IBS than those who consume a Westernized diet.
Up to 75% of adults with IBS report that diets high in refined carbohydrates, fatty foods, coffee, alcohol, and hot spices worsen their GI symptoms. Traditional diets in contrast are loaded with whole foods that contain phytonutrients which help lower inflammation and are rich in prebiotic fibres which help feed our beneficial bacteria. Traditional diets also contain fermented foods which are high in lactobacillus and bifidobacterium. Studies of both probiotics and fermented foods show that these families of good bacteria can lower the incidences of IBS.
What can I do to help my symptoms?
When it comes to diet, and reducing the incidence of IBS symptoms there are various recommendations. The initial recommendation would be to identify the ‘trigger’ foods and remove them from the diet. These would be the foods which lead to instances of IBS symptoms and foods which an individual is found to be sensitive to. Various studies have been conducted to confirm that when elimination diets are implemented, IBS symptoms are significantly reduced (8). Some studies have been conducted on the Mediterranean diet which have found to be successful in reducing the symptoms of IBS (9). The Mediterranean style of eating is a diet rich in vegetables, fruits, olive oil and fish Another common diet prescribed for IBS patients is the low FODMAP diet. A diet low in fermentable carbohydrates and polyols (10).
These are all reasonable recommendations. But only for the short-term. As I tell my clients, removing whole foods that trigger symptoms would be a short term solution. The longer term solution is to improve biodiversity of the microbiome; We need to increase resident gut bacteria, in order to begin to introduce foods that were once problematic.
In conclusion
This journey takes time, consistency and commitment. However, the journey does not require perfection. Food does not have to be avoided for life. On the contrary, if the right changes are made to diet, lifestyle and supplementation, the end goal is to begin to reintegrate foods that you love, that your IBS currently does not allow you to properly digest. There is absolute hope, it just takes time and a desire to support your health.
External resources:
1 https://www.ncbi.nlm.nih.gov/pubmed/24523597
2 https://www.ncbi.nlm.nih.gov/pubmed/22426087
3 https://www.ncbi.nlm.nih.gov/pubmed/23316916
4 https://www.ncbi.nlm.nih.gov/pubmed/24845149
5 https://www.nih.gov/news-events/news-releases/nih-human-microbiome-project-defines-normal-bacterial-makeup-body
6 https://www.ncbi.nlm.nih.gov/pubmed/23649183
7 https://www.ncbi.nlm.nih.gov/pubmed/23296252
8 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5358086/
9 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5095576/
10 https://www.ncbi.nlm.nih.gov/pubmed/29202473
May Promotions:
Probiotics – This formula from Pure Encapsulations is Lara’s recommended brand for probiotics. It contains 50 billion CFU per serving of beneficial bacteria of multiple strands in acid-resistant capsules with pH targeted release to help contribute to and maintain a healthy gut flora for optimal digestion. (Dairy and soy-free formula)

Moxa Holder Rental – Moxibustion is a similar treatment to acupuncture but stronger in its ability to improve circulation and warm the body. The moxa holder allows you to do moxibustion treatment right from your home! Just heat the moxa cones, place the holder on your navel and enjoy the treatment for about half an hour to improve your digestion. 1 month rentals with optional extensions are available.

Digestive Enzymes – Isotonix Digestive Enzymes is a powder-to-liquid formula that contains a digestive blend of a variety of enzymes including amylase, maltase and lipase. Delivered in an isotonic state, the body is able to rapidly absorb the nutrients in maximum capacity.

Lara Frendjian (RHN, CA, CPA)
Lara originally graduated from Ryerson University with a major in Accounting and a minor in Finance, and later obtained her CPA, CA designation articling with a multinational accounting firm. After experiencing the life transforming results of nutrition in her personal life, she went to obtain her Registered Holistic Nutrition designation at the Canadian School of Natural Nutrition. Read more…
Want to learn more? Book your appointment by emailing us at info@mycompletebalance.com or calling us at 416-901-2873.










Leave a Reply
You must be logged in to post a comment.